By Stacey Hooper, Senior Project Designer, HMC Architects
Healthcare facilities are caretaking entities, responsible for supporting people at their most vulnerable. Most architects and building industry professionals are aware that building sector energy reductions are crucial to minimizing greenhouse gas emissions and meeting the goals set forth by the 2030 Challenge*.The U.S. Energy Information Administration estimates healthcare buildings represent 4 percent of existing built square footage in the US, but account for 9 percent of building energy consumption. These are staggering statistics for a building industry that consumes 48.7 percent of energy produced in the United States. Creating a balance between energy reductions and sustaining a healing environment requires genuine commitment and a nuanced understanding of all the variables defining a high-performance, care-taking facility.
*HMC Architects is an adopter of the 2030 challenge. In 2011, HMC reported an average Predicted Energy use Intensity reduction of 36.1%.
Understanding the Variables
Evidence-based design studies confirm the healing benefits between natural light and patient views of natural settings resulting in shortened hospital stays. Roger Ulrich first substantiated this correlation in his landmark study, “View through a Window May Influence Recovery from Surgery.” More recent studies speak to the benefits of connection to the diurnal cycles of day and night, which naturally keep our circadian rhythms in check. Access to daylight has also been linked to improving mental health and dementia, promoting healthy sleep patterns, and supporting our overall health and physiological function. Moreover, exposure to sunlight provides healthy doses of vitamins A and D. The true benefits may be immeasurable.

High-performance building envelopes can’t be considered without a holistic evaluation of integrated building systems and their relationship to life cycle costs and wellness priorities. For example, a more passive mechanical system, such as displacement ventilation, can provide significant energy reduction. However, it may require more aggressive exterior shading strategies, which in turn affect views and day lighting solutions. It may also require higher first costs, but the energy saved, possibly in excess of 45 percent over code, can result in significant paybacks, possibly in less than two years*. This exemplifies the complex balancing act faced by designers, required for measuring the success of high-performance healthcare facilities.
The first step towards significant energy reduction in healthcare buildings is to target more efficient and innovative mechanical systems and central plants. These building types are typically internal loaded versus external loaded buildings. An internal loaded building’s function and occupancy requires higher air changes by code and produces heat that drives a predominantly air-conditioned environment. In an external loaded building, temperatures fluctuate in the relative heat gain and loss through the building envelope. This is a critical differentiator, since the contribution of the envelope relative to energy reduction becomes more limited for an externally loaded building. Also of importance are strategies that provide better infection control and comfort. By way of example, selecting a displacement ventilation system with 100 percent outside air reduces energy, provides reduced infection rates by improving IAQ (Indoor Air Quality) within the breathing zone, and increases patient comfort by eliminating uncomfortable drafts. The remaining energy load is a mix of equipment load, plug load, lighting, and building envelope performance.
A Case for High-Performance Design
The building envelope is central to supporting overall patient comfort and meeting energy reduction goals. An optimally reduced peak load through the envelope design can cut back as much as 10 percent of the total energy use. These integrated sustainable solutions rely heavily on the performance of the building envelope to balance temperature fluctuation, especially within the first 15 feet of the building envelope, primarily patient rooms. This is where heat gain and loss through the envelope most affect the well-being and comfort of the building’s occupants.

Patient rooms at this private medical center have ample windows with “shades down” option for privacy.
The default strategy in tackling envelope performance is to reduce glazing to small punched openings and increase insulated, solid wall area at patient rooms. This does not support the previously mentioned research, or take into consideration the big picture. The quality of the view relative to glare is exacerbated by the use of punched openings (due to contrast between solid wall area and the brightness of the glazed area). This can also result in an interior shades down scenario a large percentage of the year, where patients may be reliant on their caretakers to control their access to the view as the day progresses. Even if motorized shades are provided, the need to have the shades down due to poor design and uncontrolled glare defeats the good intention of providing window openings to connect patients with the outdoors. Unless clerestories are provided, shades down may also adversely affect the natural day lighting to the patient room, creating an increased electric lighting demand. The solution is to design ample window openings. What is “ample” can be nebulous without a thorough view-oriented study. At a minimum, the building should comply with the Green Guide for Health Care.
Shading design should optimize performance of view windows, requiring a studied balance between glass selection, exterior shading and interior shades. Ideally, exterior shading devices control heat gain and glare and interior shades control privacy. Exterior shading devices must also be designed with consideration for obstructions within the line of sight, such as a view out to the horizon or to the sky. These fixed shading obstructions are often referred to as “visual noise.” Motorized exterior shades versus exterior fixed shading systems can provide ultimate flexibility and the highest performance, but have the challenge of higher first cost and often difficult to justify through life-cycle analysis.
So what is the answer?
Simply put, the answer is good, responsive, considerate design. It requires a committed, creative and tested balance weighing the following:
• Energy Goals
• Building Shape, Volume, and Orientation
• Climate
• Fenestration and Shading Strategies
• Air and Moisture Control
• Operations and Maintenance
• Thermal Efficiency
• Building Material Selection and Properties
• User Control and Flexibility
• First Cost/Life-Cycle Cost
Each of these variables warrants a full explanation of the unique contribution, but optimizing these strategies further reinforces healthy daylighting solutions. These solutions reduce electric light loads, maintain a view and connection to the outdoors free from glare and visual noise, and provide varying degrees of user control.
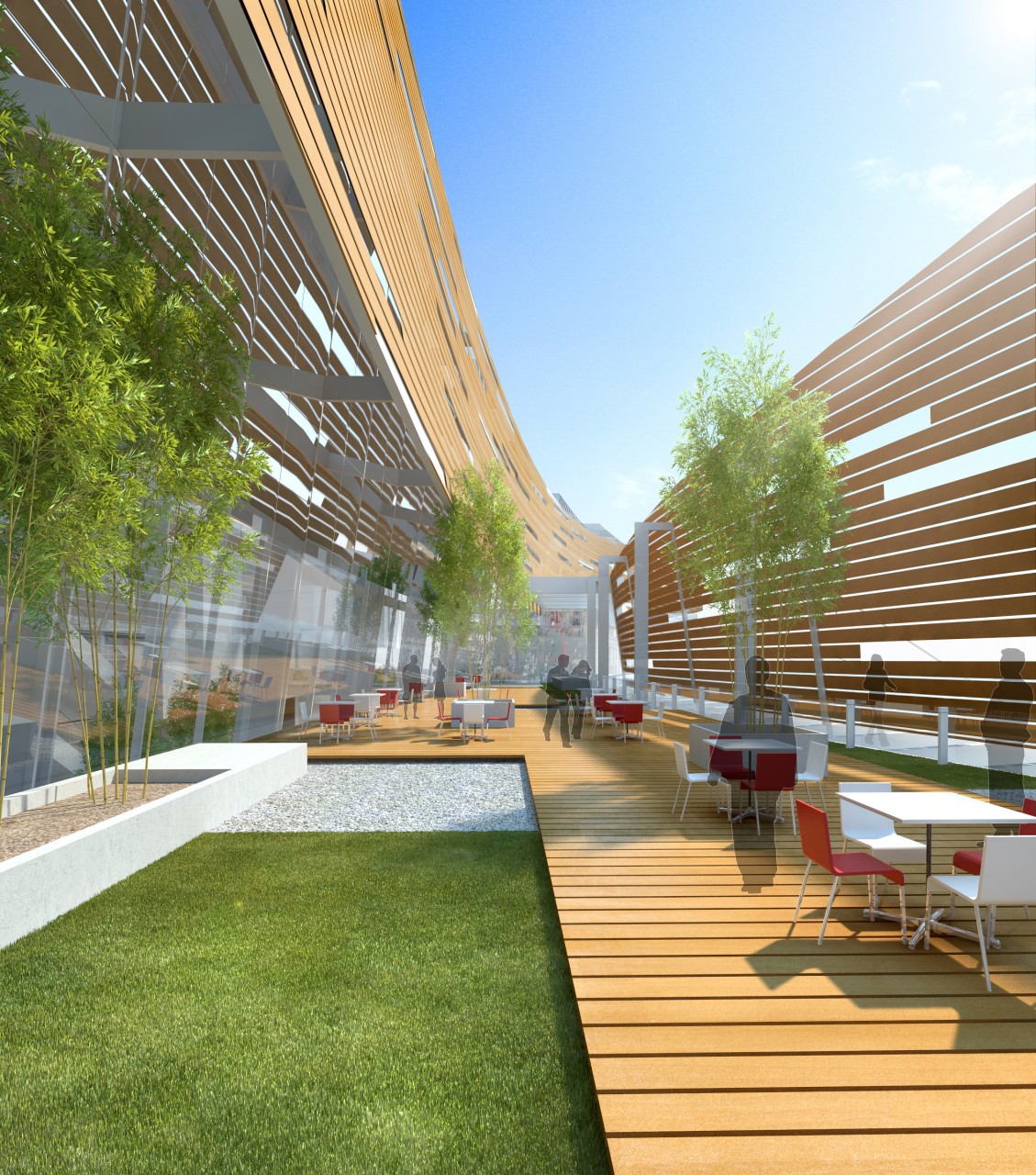
Although we focused on the connection between building systems and the envelope, primarily at perimeter patient rooms, the same principles apply to supporting staff and visiting families. A high-performance strategy is good for users, facilities, and the planet alike. Aspiring to meet these goals supports the wellness and spirit of the human experience we all share.
*Energy Star estimates that for “every $1 a non-profit healthcare organization saves on energy is equivalent to $20 in new revenues,” and for-profit hospitals can “boost earnings per share by a penny by reducing energy costs just 5 percent.”
