In today’s rapidly evolving healthcare environment, where the pursuit of optimal patient outcomes meets the imperative to maximize resource efficiency, innovation becomes the linchpin of progress. In this realm, a visionary approach beckons us to bridge two fundamental pillars of medical care: surgical and interventional platforms. By weaving together these traditionally distinct domains into a seamless, consolidated powerhouse, we can unlock the potential for unparalleled synergy. This integrated approach promises to elevate patient care, charting a course toward improved cost-effectiveness and cultivating a collaborative learning environment within healthcare organizations. This article marks the beginning of a two-part series on the evolution of operating rooms (ORs), with the second part focusing on renovation projects.
Historical Evolution of Interventional Procedures
The birth of Interventional Procedures (INTP) marked a paradigm shift in the medical field, ushering in a new era of minimally invasive treatments. Emerging from diagnostic radiology, this innovation was made possible through the relentless evolution of technology. INTP allowed real-time treatment during diagnosis by utilizing needles, wires, and catheters, bridging the gap between identification and intervention. This groundbreaking approach, rooted in imaging guidance, enables precision cuts and fewer incisions, drastically improving patient outcomes.
Traditional Surgical Operating Room Platforms
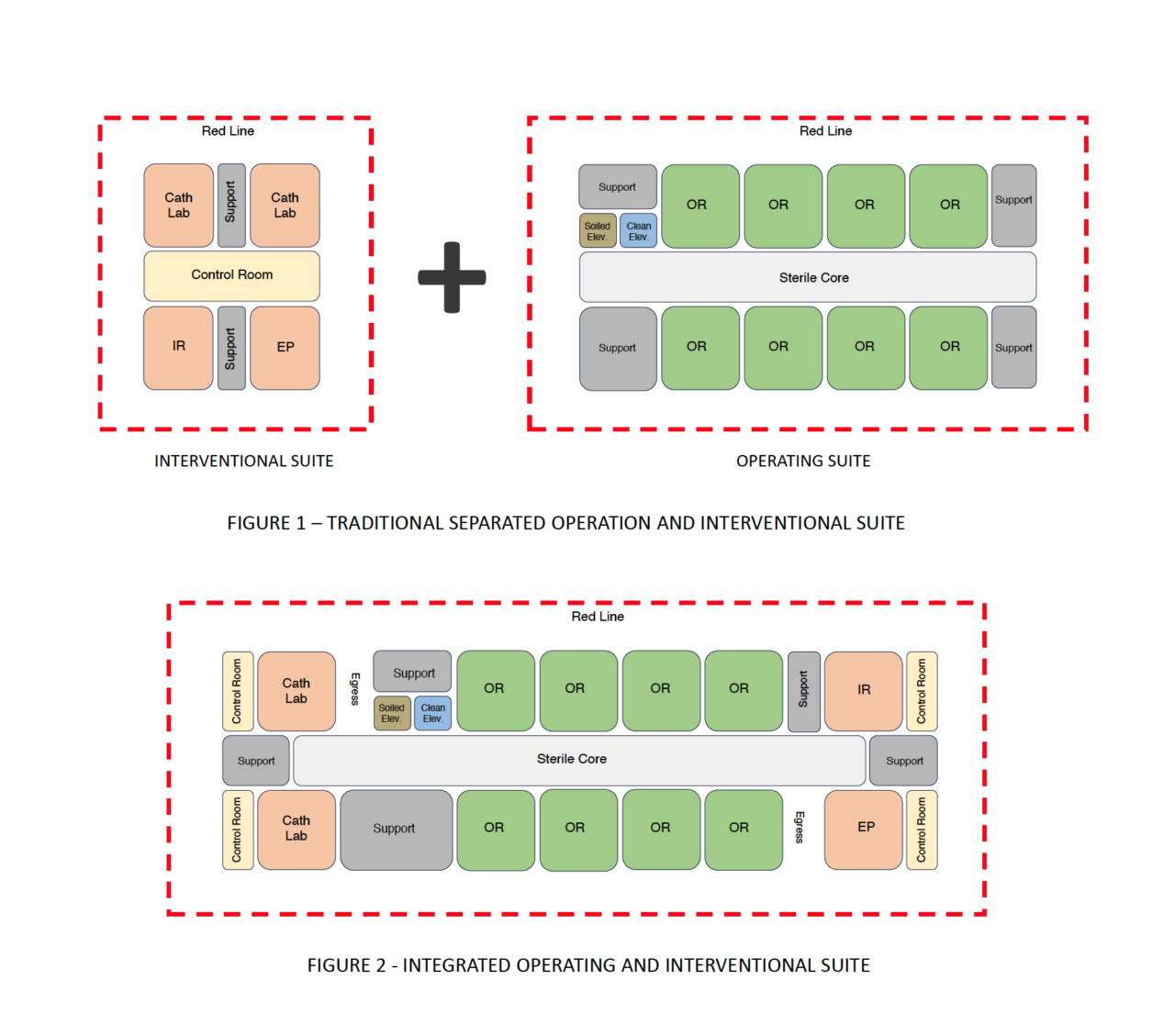
The history of operating rooms (ORs) is deeply entrenched, with roots dating back to the Middle Ages. Modern OR platforms have evolved to emphasize centralized sterile cores and infection control. These platforms incorporate clean and soiled elevators, often directly connected to Sterile Processing Services (SPS), ensuring efficient supply delivery and infection prevention. Controlled access points regulate medical staff movement, enhancing patient safety and maintaining strict hygiene standards.
The Converging Trajectories of Surgical and Interventional Platforms
The operational flow of Interventional Procedures bears a striking resemblance to that of traditional surgeries. Over time, there has been a growing demand for perioperative services and sterile supply delivery within INTP. Contrary to traditional settings, there is no inherent reason for separating Interventional Procedures from surgical platforms geographically. Integration is key, as the complexity of treatments transforms the dynamics between diagnosis and perioperative care.
Challenges of Traditional Settings and the Call for Consolidation
Historically, healthcare facilities have operated within silos, impeding the potential for comprehensive care delivery. Transitioning to consolidated platforms requires a shift in mindset, embracing optimized models and fostering a culture of collaboration. This shift necessitates reevaluating healthcare business models to enhance quality, efficiency, and accessibility. A consolidated Surgical and Interventional platform addresses this challenge, offering a cost-effective solution while streamlining operational workflows.
The Benefits of a Consolidated Approach
The adoption of consolidated Surgical and Interventional platforms holds immense promise, delivering a multitude of benefits for healthcare organizations and patients alike:
- Cost Savings: A single location for both platforms results in efficient staffing and shared resources, translating to substantial operational cost savings.
- Resource Optimization: Shared resources and cross-training opportunities lead to optimized staff utilization and enhanced skill development.
- Maximized Utilization: Utilization rates are maximized through streamlined processes and eliminating redundant spaces.
- Collaborative Learning: Consolidation fosters a collaborative learning environment, enabling surgeons and interventionists to cross-train and broaden their skill sets.
- Simplified Patient Journey: Centralized platforms minimize patient transportation, enhancing patient satisfaction and ease of care.
- Infection Control: A consolidated platform linked to a sterile core ensures consistent infection control measures and facilitates monitoring.
- Efficient Logistics: Streamlined logistics and auxiliary services enhance the management of supplies, instruments, and equipment.
Integrating surgical and interventional platforms represents a visionary and transformative approach in today’s healthcare landscape. This consolidation offers numerous benefits, including cost savings, resource optimization, collaborative learning, and streamlined patient care. Adopting such a consolidated approach enhances operational efficiency and fosters a culture of collaboration and innovation within healthcare organizations. By seamlessly integrating disciplines, optimizing resource utilization, and enhancing patient outcomes, this approach exemplifies the ongoing dedication of healthcare professionals to delivering the highest standards of care.
